Vision includes many aspects, such as visual acuity, color vision, stereoscopic vision, and form vision. Currently, various defocused lenses are mainly used for myopia correction in children and adolescents, requiring accurate refraction. In this issue, we will briefly introduce the accuracy of myopia correction in children and adolescents, focusing on the minimum degree of best vision in the refractive prescription to help us select appropriate optical lenses.

The minimum degree of best vision needs to be carefully analyzed to determine when it is appropriate to correct vision to 1.5 and when it is more suitable to correct vision below 1.5. This involves understanding which situations require accurate refraction and which situations may tolerate undercorrection. The definition of best vision should also be clarified.

Defining the criteria for visual acuity standards
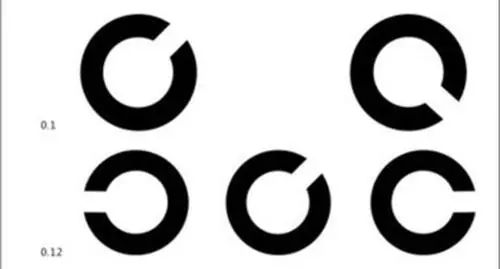
Usually, when people talk about visual acuity, they are referring to form vision, which is the ability of the eyes to distinguish external objects. In clinical practice, visual acuity is primarily assessed using a visual acuity chart. In the past, the main charts used were the international standard visual acuity chart or decimal visual acuity chart. Currently, the logarithmic letter visual acuity chart is commonly used, while certain specialized professions may require a C-type visual acuity chart. Regardless of the type of chart used, visual acuity is typically tested from 0.1 to 1.5, with the logarithmic visual acuity chart ranging from 0.1 to 2.0.
When the eye can see up to 1.0, it is considered standard visual acuity. While most people can see up to 1.0, there is a small percentage of individuals who can exceed this level. A very small number of individuals can even see as clearly as 2.0, with research in laboratories suggesting that the best visual acuity may reach 3.0. However, clinical assessment typically considers 1.0 as the standard visual acuity, which is commonly referred to as normal vision.
1 Measurement Distance
The 'Standard Logarithmic Visual Acuity Chart' stipulates that the examination distance is 5 meters.
2 Testing Environment
The visual acuity chart should be hung in a well-lit area, with its height aligned so that the line marked '0' on the chart is at the same level as the examinee's eyes. The examinee should be positioned 5 meters away from the chart, facing away from the light source to avoid direct light entering the eyes.

3 Measurement Method
Each eye should be tested separately, starting with the right eye followed by the left eye. When testing one eye, the other eye should be covered with an opaque material without applying pressure. If the examinee can only read up to the 6th line clearly, it is recorded as 4.6 (0.4); if they can read the 7th line clearly, it is recorded as 4.7 (0.5), and so on.
The minimum line of visual acuity that the examinee can identify should be noted (the examinee's visual acuity is confirmed to reach that value when the correctly identified number of optotypes exceeds half of the total number of optotypes in the corresponding row). The value of that line is recorded as the visual acuity of that eye.
If the examinee cannot clearly see the letter 'E' on the first line of the chart with one eye, they should be asked to move forward until they can see it clearly. If they can see it clearly at 4 meters, their visual acuity is 0.08; at 3 meters, it is 0.06; at 2 meters, it is 0.04; at 1 meter, it is 0.02. A single-eye visual acuity of 5.0 (1.0) or above is considered normal visual acuity.
4 Examinee's Age
Generally, the refractive development of the human eye progresses from farsightedness to emmetropia and then to nearsightedness. With normal accommodative reserves, a child's uncorrected visual acuity is around 0.5 at 4-5 years old, around 0.6 at 6 years old, around 0.7 at 7 years old, and around 0.8 at 8 years old. However, each child's eye condition varies, and calculations should be made according to individual differences.

It is important to note that a single-eye visual acuity of 5.0 (1.0) or above is considered normal visual acuity. Normal visual acuity does not necessarily represent the examinee's best vision.

Different Refractive Needs at Different Ages
1 Adolescents (6-18 years old)
An expert mentioned, "Undercorrection can easily lead to an increase in diopter. Therefore, adolescents must have appropriate correction."
Many optometrists used to provide slightly lower prescriptions, known as undercorrection, when conducting eye exams for myopic children and adolescents. They believed that compared to full correction prescriptions, undercorrection prescriptions were more easily accepted by parents, as parents were reluctant to have their children wear high-powered glasses, fearing that the diopter would increase faster, and worried that the glasses would become a permanent necessity. Optometrists also thought that wearing undercorrected glasses would slow down the progression of myopia.
Undercorrection for myopia refers to wearing glasses with a lower prescription than normal, resulting in corrected visual acuity below the normal 1.0 level (while not achieving optimal visual acuity standards). The binocular visual function of children and adolescents is in an unstable stage and clear vision is necessary to maintain the stable development of their binocular vision function.
Wearing undercorrected glasses not only hinders the ability to see objects clearly in children and adolescents but also impedes the healthy development of vision. When viewing near objects, less accommodation and convergence power than normal are used, leading to a decrease in binocular visual function over time, causing visual fatigue, and accelerating myopia progression.
Children not only need to wear appropriately corrected glasses but also, if their visual function is poor, they may need vision training to improve their eye's focusing ability to alleviate eye fatigue and slow down the progression of myopia caused by abnormal focusing function. This helps children achieve clear, comfortable, and sustained visual quality.

2 Young Adults (19-40 years old)
In theory, myopia levels in this age group are relatively stable, with a slow progression rate. However, due to environmental factors, individuals who spend long periods using electronic devices are prone to further exacerbating their myopia levels. In principle, the lowest necessary prescription to achieve optimal vision should be the main consideration, but adjustments may be made based on customer comfort and visual needs.
Points to Note:
(1) If a significant increase in diopter is observed during an eye exam, the initial increase in prescription should not exceed -1.00D. Pay attention to discomfort symptoms such as walking, distortion of the ground surface, dizziness, clarity of near vision, eye soreness, distortion of electronic device screens, etc. If these symptoms persist after wearing the glasses for 5 minutes, consider reducing the prescription until it is comfortable.
(2) For individuals with high-demand tasks such as driving or viewing presentations, and if the customer is comfortable with full correction, it is advisable to use the appropriate correction. If there is frequent close-up use of electronic devices, consider using digital lenses.
(3) In cases of sudden worsening of myopia, be mindful of accommodative spasm (pseudo-myopia) possibilities. During eye examinations, confirm the lowest necessary prescription for optimal visual acuity in both eyes, avoiding overcorrection. If there are issues with poor or unstable corrected visual acuity, consider conducting relevant visual function tests."

3 Elderly Population (40 years and above)
Due to the decline in the eye's accommodation ability, this age group often experiences presbyopia. Besides focusing on the prescription for distance vision, it is important to pay special attention to the near vision correction when prescribing glasses for this age group and consider the customer's adaptability to prescription changes.
Points to Note:
(1) If individuals feel that their current prescription is insufficient and have a higher demand for distance vision, after confirming the prescription for distance vision, it is crucial to check the near vision. If there are symptoms of visual fatigue or a decline in near vision due to decreased accommodation ability, consider prescribing a pair of progressive multifocal lenses.
(2) Adaptability is lower in this age group. Ensure that each increase in nearsightedness prescription does not exceed -1.00D. If discomfort persists after wearing the glasses for 5 minutes, consider reducing the prescription until it is comfortable.
(3) For individuals over 60 years old, there may be varying degrees of cataracts present. If there is a deviation in corrected visual acuity (<0.5), suspect the possibility of cataracts in the customer. Detailed examination at a hospital is necessary to rule out the influence of ophthalmic diseases.

Impact of Binocular Vision Function
We know that the results obtained from an eye examination reflect the refractive state of the eyes at that time, which generally ensures clear vision at the examination distance. In normal daily activities, when we need to see objects at different distances, we require adjustment and convergence-divergence (the involvement of binocular vision function). Even with the same refractive power, different states of binocular vision function require different correction methods.

We can simplify common binocular vision abnormalities into three categories:
1 Ocular deviation - Exophoria
Corresponding abnormalities in binocular vision function may include: insufficient convergence, excessive divergence, and simple exophoria.
The principle for such cases is to use adequate correction and to complement it with visual training to improve the convergence ability of both eyes and alleviate visual fatigue caused by binocular vision abnormalities.
2 Ocular deviation - Esophoria
Corresponding abnormalities in binocular vision function may include: excessive convergence, insufficient divergence, and simple esophoria.
For such cases, the principle is to consider under-correction while ensuring adequate vision. If near vision tasks are frequent, digital lenses can be used. Additionally, complementing with visual training to improve the divergence ability of both eyes can help alleviate visual fatigue resulting from binocular vision abnormalities.
3 Accommodation anomalies
Mainly include: Insufficient accommodation, excessive accommodation, accommodation dysfunction.

1 Insufficient Accommodation
If it is myopia, avoid overcorrection, prioritize comfort, and consider under-correction based on the trial wearing situation; if it is hyperopia, try to fully correct the hyperopic prescription as much as possible without affecting clarity.
2 Excessive Accommodation
For myopia, if the lowest negative spherical lens for best vision cannot be tolerated, consider under-correction, especially for adults who primarily engage in prolonged near work. If it is hyperopia, try to fully correct the prescription without affecting clarity.
3 Accommodation Dysfunction
For myopia, if the lowest negative spherical lens for best vision cannot be tolerated, consider under-correction. If it is hyperopia, try to fully correct the prescription without affecting clarity.

In Conclusion
When it comes to optometric principles, we need to consider a comprehensive range of factors. While taking age into account, we must also consider binocular vision function. Of course, there are special cases such as strabismus, amblyopia, and refractive anisometropia that require separate consideration. Under different circumstances, achieving the best vision challenges the technical skills of every optometrist. We believe that with further learning, every optometrist can comprehensively assess and provide accurate prescription data.

Post time: Jul-04-2024

